Communication for Safe Care: About
What is the Communication for Safe Care Project?
We are making healthcare services more accessible for people with communication support needs. We are working with Health Care Workers and people with communication support needs to co-design solutions to existing barriers.
Why are we doing this project?
An estimated 1.2 million Australians present with communication difficulties (ABS, 2015). Communication breakdowns in health care settings can result in errors, misdiagnosis, inappropriate treatment, and poor care outcomes.
Health care workers report high levels of compassionate care. They want to help patients with communication support needs, but often lack the knowledge and confidence to do so. Health Care workers are often working in environments where patient-provider communication is often not adequately resourced (Carragher et al, 2020).
Co-designing communication accessible healthcare services will help both patients and staff.
People with communication support needs may:
-
Be better understood by healthcare professionals
-
Feel safer and more included
-
Have greater choice and control over their own health care
The project will enable healthcare services to:
-
Deliver safe, timely and high-quality care for people with communication support needs
-
Improve staff skills
-
Increase staff confidence and satisfaction.
What are communication support needs?
Communication support needs may include difficulties at any point of the communication pathway: giving, receiving, processing, or understanding information.
People with communication support needs may have:
-
Intellectual disability
-
Neurological injury
-
Autism
-
Communication disorders
-
Psychosocial disability
-
Sensory disability (such as blindness, low vision, hearing loss)
What is communication access?
Communication looks different for every person! Communication access means that everyone can get their message across and be understood.
We are aiming to improve communication between people and health care services. We are looking at this holistically from environmental design to day-to-day interactions between health care workers and consumers. Watch this video to find out more.
Who is involved in the Communication for Safe Care project?
The Communication for Safe Care project has partnered with four key NSW Health sites:
-
A metropolitan Emergency Department
-
A metropolitan Oral Health Service
-
A regional Oral Health Service
-
A regional Perioperative Service
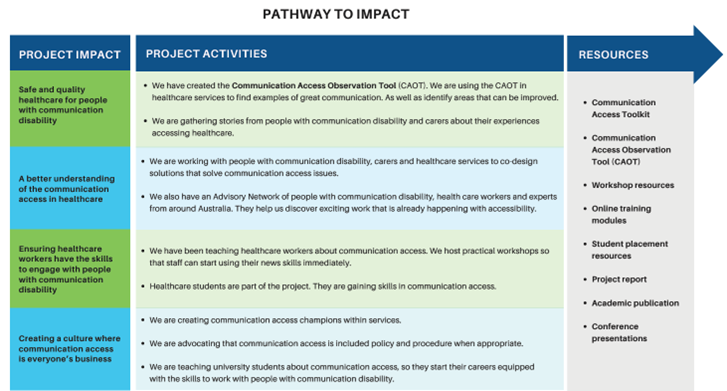
How are we creating change?
The Communication for Safe Care project aims to:
-
Deliver safe and quality healthcare
-
Understand local context and healthcare environments
-
Build current and future healthcare worker capacity and skills
-
Transform the culture of healthcare services
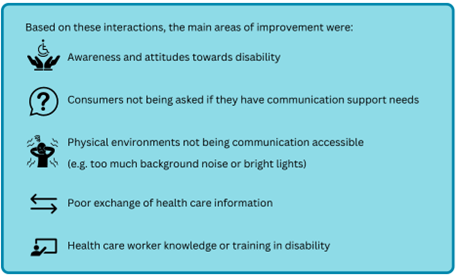
Barriers and facilitators to communication
We gathered information about the barriers and facilitators for communication in healthcare services.
We talked to people with communication support needs, carers, health care workers and support staff.
The main areas to focus on improving were:
-
Awareness and attitudes towards disability
-
Consumers not being asked if they have communication support needs
-
Physical environments not being communication accessible (e.g., too much background noise or bright lights)
-
Poor exchange of health care information
-
Health care worker knowledge or training in disability
Developing solutions
We have completed workshops with healthcare workers, consumers, and senior leaders at each target site.
In these workshops, the project team supported participants to work together and brainstorm solutions to improve access to health care for people with communication support needs.
The project team are developing these solutions and working with the target sites to implement change. Stay tuned for updates as we progress towards a more inclusive healthcare environment.

Acknowledgements:
We would like to acknowledge the original funding application authors: Dr. Katherine Kelly, Lisa Maxey and Prof. Sue McAllister.
We would like to also acknowledge members of the Project Advisory Committee, which includes people with lived experience of communication disability and industry.
|
Project Members – NSW Health |
|
Dr Katherine Kelly – Disability and NDIS Coordinator, South Western Sydney Local Health District Ms Merryn John – Disability Strategy Manager, Western NSW Local Health District Ms Nicole Chapman – Project Manager, South Western Sydney Local Health District Ms Alyssa Walter – Project Officer, Western NSW Local Health District Ms Arianne Tan – Project Officer, Western NSW Local Health District Ms Lana Micallef – Project Officer, South Western Sydney Local Health District Ms Rae Anne Carorasan – Clinical Specialist, South Western Sydney Local Health District |
|
Project Members – University of Sydney |
|
Prof. Sue McAllister – Project Advisor Prof. Sarah Dennis – Professor Allied Health, Sydney School of Health Sciences Dr. Iqbal Hassan – Research and Evaluation Officer A/Prof Gillian Nisbet – Director of Partnerships and Placements, Sydney School of Health Sciences Dr. Elizabeth Bourne – Program Director of Masters of Speech Pathology & Work Integrated Learning Placement Innovation Lead Dr. Robyn Johnson – Health Professions Education Lead (Speech Pathology) A/Prof Anya Johnson – Deputy Head of Discipline, Work and Organisational Studies, Sydney Business School. Dr. Ju Li Ng – Deputy Director for Master HRM and IR, Work and Organisational Studies, Sydney Business School Prof Leanne Togher – Professor Communication Disorders after TBI & Senior NHMRC Research Fellow Dr. Elise Elbourn – Lecturer (Neurogenic Language Disorders and Language), Sydney School of Health Sciences Dr. Rachael Rietdjik – Lecturer, Speech Pathology, Sydney School of Health Sciences Dr. Melissa (Liss) Brunner – Lecturer, Speech Pathology, Sydney School of Health Sciences |
|
Project Members – Associate Investigators |
|
Ms Fiona Murphy Ms Katherine Shannon Ms Karri Kneebone Ms Rebecca Karmas Ms Molly Banks |
References:
Australian Bureau of Statistics (ABS). (2015). Disability and carers, Australia: Summary of findings, 2015. (No.4430.0). https://www.abs.gov.au/ausstats/[email protected]/Previousproducts/4430.0Main%20Features982015?opendocument&tabname=Summary&prodno=4430.0&issue=2015&num=&view=
Bartlett, G., Blais, R., Tamblyn, R., Clermont, R.J., & MacGibbon, B. (2008). Impact of patient communication problems on the risk of preventable adverse events in acute care settings. Canadian Medical Association Journal, 178(12), 1555-1562. https://doi.org/10.1503/cmaj.070690 Carragher, M., Steel, G., O’Halloran, R., Torabi, T., Johnson, H., Taylor, N. F., & Rose, M. (2020). Aphasia disrupts usual care: the stroke team’s perceptions of delivering healthcare to patients with aphasia. Disability and Rehabilitation, 1-12. https://doi.org/10.1080/09638288.2020.1722264